Emergency Department Applications
|
Computed Tomography (CT) of the Head
CT scanning has replaced most other modalities of imaging in the acute evaluation of neurologic injury or disease. No longer are we taught to look for pineal gland calcification on skull film as a way of detecting midline shift, nor do we order plain skull films to identify skull fractures, when what we are really concerned about is
underlying brain injury. (Although there may still be a role for skull films in selected cases.)
As CT technology has evolved, so has the acute treatment of many neurologic illnesses. Neurologic injuries or illnesses are typically time-sensitive diagnoses, much as myocardial infarction, with survival dependent on time to treatment. A good example of this is treatment of subdural hematoma, whose mortality goes from 90%
to 30% if operative treatment is within 4 h. Rapid, available and accurate CT scanning is no longer the property of tertiary academic centers but now ubiquitous throughout the healthcare landscape. For this reason, it is important for everyone to understand the utility and limitations of the technology.
This chapter will review the utility of CT scan in selected diagnoses and touch on some of the pitfalls associated with each. The value of magnetic resonance imaging (MRI) will be discussed in a separate section.
CT in Nontraumatic Conditions
Subarachnoid Hemorrhage (SAH)
- CT preferred over MRI for acute SAH
- Detects over 90% within 24 h. (corollary is that 10% are missed)
- May become negative after 3 days with change in blood density.
- Etiology most commonly aneurysmal.
- Lumbar puncture required to rule out acute SAH after negative CT scan.
- Findings include blood in the sulci, interpeduncular cisterns, sylvian fissures, or posterior falx cerebri.
- Pitfalls:
- Failure to perform lumber puncture after negative head CT to rule out occult SAH (false negative rate up to 5% with CT alone.)
- CT scan will be negative after 3 days, but lumbar puncture shows xanthochromia.
- Sensitivity may be decreased in setting of anemia.
Cerebral Vascular Accident (CVA)
- May not be evident on initial scan within 24 h.
- Early signs include hyper-dense artery (usually MCA distribution) due to thrombus in the artery, loss of basal ganglia, loss of grey-white border distinction.
- Subacute stroke will often show slight mass effect.
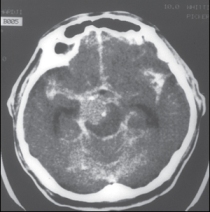
Figure: Subarachnoid Hemorrhage.
Note the bright signal of the subarachnoid hemorrhage collecting in the sulci and cisterns.
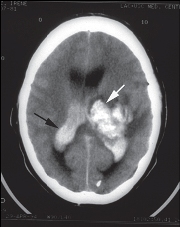
Figure: Hemorrhagic basal ganglia cerebral vascular accident (white arrow)
with rupture into ventricular space (black arrow).
- Subacute to chronic CVA will gradually become hypo-dense to normal brain tissue.
- Acutely, CT scan is primarily useful to rule out associated hemorrhage or other stroke mimics, such as subdural hematoma, tumor, etc.
- Nontraumatic hemorrhagic CVA most commonly hypertensive in etiology with the following locations most common:
- Putamen
- Thalamus
- Pons
- Cerebellum
- Pitfalls in CVA:
- Acute CVA may not be evident on CT within 24 h.
- Cerebellar anatomy not clearly visualized on CT and may require thin cuts through the posterior fossa or MRI.
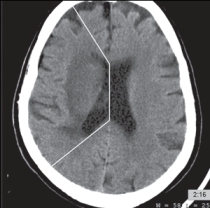
Figure: Right middle cerebral artery territory cerebral vascular accident. Note the edema and loss of gray-white junction seen in the highlighted area.
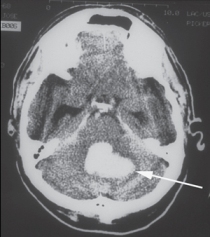
Figure: Cerebellar hemorrhage.
Infectious Processes
Toxoplasmosis
- Seen in AIDS or other immunocompromising illnesses.
- Most commonly focal, but may be diffuse.
- Focal disease ring enhanced with intravenous contrast.
- Commonly found at basal ganglia and gray-white border of the cerebral hemispheres.
- Differential includes lymphoma and may be impossible to distinguish without biopsy or empiric treatment for Toxoplasmosis.
Cysticercosis
Hydrocephalus
Trauma
Epidural Hematoma
- Collection of blood in the potential space between the dura and skull. It is most commonly found in the temporal region and most often has an overlying skull fracture.
This type of injury has a better prognosis (90% survival) than subdural because the skull has often absorbed the majority of the force involved. The epidural hematoma has distinct characteristics based on its pathophysiology:
- It is lenticular (lens shaped) in form as it separates the dura from the skull.
- It does not cross suture lines as the dura is attached to the skull at these points.
- It has an associated fracture in 95% of cases seen on the bone windows of CT.
- It may exhibit “swirling”, an inhomogeneous appearance of the bleed, due to active arterial bleeding within the epidural hematoma.
- Less common in infants and the elderly as the dura is firmly attached in both these populations.
- Pitfalls in epidural hematoma:
- Failure to diagnose small epidural which can either expand or rebleed, causing neurologic deterioration.
- Obtaining the CT scan too early. Really. Although an uncommon problem, especially in inner-city hospitals, a CT scan obtained too quickly may not detect small epidural hematomas, which can expand and cause secondary brain injury.
- Subdural hematoma:
- Collection of blood in the potential space between the dura and the pia mater. The source of bleeding is usually due to the bridging veins as they empty in the dural sinuses. Subdural hematomas may occur without direct head injury in the case of severe acceleration/deceleration injury. Subdural hematoma has a 30% mortality

Figure: Epidural hematoma. The lenticular-shaped hemorrhage is seen in the left temporal-occipital region.

Figure: Underlying temporal skull fracture associated with the above epidural hematoma.
rate (with appropriate treatment) since underlying brain injury is both common and severe.
- Characteristics of subdural hematoma on CT scan include:
- Crescent shaped.
- Confined by dural attachments at the midline.
- May be acute, subacute or acute and chronic.
- May show a hematocrit effect, where the red cells settle from the serum and produce a fluid level on the CT scan. This occurs in a patient who remains supine for a prolonged period of time.
- Pitfalls in subdural hematoma:
- A small subdural may only appear as increased density of the tentorium as the subdural blood tracks along it.
- Failure to recognize the iso-dense subdural. Often the only clues may be subtle mass effect or loss of sulci on the side of the subdural.
- Failure to recognize bilateral injuries. Subdurals will be bilateral in 15% of cases, and with iso-dense or chronic blood the diagnosis can be very difficult.
- As mentioned above, the appearance of blood will change on CT scan depending on age of the bleed. This differentiation is clinically helpful in determining age of injury.

Figure: Acute subdural hematoma.
A right frontal-temporal subdural hematoma with midline shift is demonstrated in this CT scan of a fall victim.

Figure: Chronic subdural hematoma.
A left chronic (hypo-dense) subdural with midline shift is seen on this CT.
Table Comparison of CT findings of EDH and SDH
| Finding |
EDH |
SDH |
| Shape: |
Lenticular |
Crescent |
| Bleed confined to: |
Will not cross suture lines |
Will not cross midline falx |
| Source of bleed: |
Arterial (may see swirling) |
Venous |
| Skull fracture associated: |
Yes |
No |
| Rebleed: |
Yes |
Less common |
- Acute blood (< 7 days) is hyper-dense to the brain tissue and often easily recognizable.
- Subacute blood (between 7 days and 3 wk) is often iso-dense with the brain tissue and has subtle findings of mass effect on CT.
- Chronic blood (over 3 wk of age) will be hypo-dense in comparison with brain tissue.
Other Injuries
Diffuse Axonal Injury (DAI)
- Though patients usually present clinically in deep coma, the CT scan is often normal in appearance (70-80%).
- This type of shearing injury leads to disruption of the grey-white border, corpus callosum or brainstem. This accounts for the profound neurologic deficits. Unless there are associated small hemorrhages, the initial CT scan may reveal no abnormality.
- MRI is sensitive for the detection of diffuse axonal injury, though not often available or practical in the acute poly-trauma patient.
Skull Fractures
- Skull fractures are readily identified on the bone windows of CT scan, but small non-displaced linear skull fractures may be missed on CT. Most nondisplaced fractures are not clinically significant but for underlying brain injury.
- Skull fractures depressed more than one bony table width may require elevation and are more often associated with underlying injuries.
- Basilar skull fractures are the exception to CT sensitivity. The clinical exam is still more reliable than CT scan in the detection of basilar skull fractures. Clinical signs include:
- Raccoon eyes: bruising of the eyelids sparing the tarsal plate, signifying bleeding tracking from behind the orbits rather than direct trauma.
- Battle’s sign: bruising of the mastoid due to associated fracture. This sign may be delayed up to 48 h and is not reliable in excluding fracture.
- Hemotympanum: Blood behind the tympanic membrane is seen immediately after basilar skull fracture.
- CSF leak: either otorrhea or rhinorrhea may be associated with basilar skull fracture and may lead to meningitis. Prophylactic antibiotics are not usually recommended but remain controversial.
- Cranial nerve deficits: Look for cranial nerve deficits of the facial, auditory or trigeminal or ophthalmic nerves.
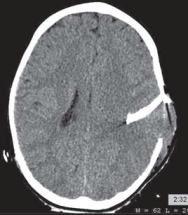
Figure: Left temporal depressed skull fracture on CT.
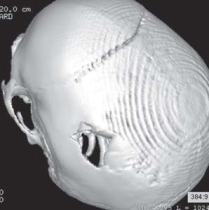
Figure: Three dimensional reconstruction of the same temporal skull fracture

Figure: Pneumocephalus appears as black space on CT scan. This should prompt a search for an underlying basilar skull or sinus fracture.
|